What Is Gram Negative Bacteria & Why Can It Cause So Many Diseases
What is Gram-Negative bacteria?
Gram-negative bacteria are a diverse group of microorganisms characterized by their unique cell wall structure. They stain pink or red when subjected to the Gram stain test, indicating the presence of a thin peptidoglycan layer sandwiched between two cell membranes. This structural distinction plays a significant role in their ability to cause a wide range of diseases.
Gram-negative bacteria have adapted to various environments and can be found in soil, water, plants, and animals, including humans. Their versatility and adaptability contribute to their ability to cause a multitude of diseases. Some notable examples of Gram-negative bacteria include Escherichia coli (E. coli), Salmonella spp., Pseudomonas aeruginosa, Klebsiella pneumoniae, and Neisseria gonorrhoeae.
Figure 1: Gram-negative bacteria under the microscope
Key Takeaways
- Their distinct cell wall composition affects disease mechanisms.
- Gram-negative bacteria produce endotoxins and possess virulence factors.
- Antibiotic resistance poses challenges in treatment.
- They cause diseases such as UTIs, gastrointestinal infections, pneumonia, and hospital-acquired infections.
- Prevention involves hygiene, proper wound care, balanced diet, and food safety practices.
Gram-Negative Bacteria Vs. Gram-Positive Bacteria
Gram-negative and Gram-positive bacteria are two broad categories based on their response to the Gram staining technique, which helps differentiate them based on their cell wall structure.
| Characteristic | Gram-Negative Bacteria | Gram-Positive Bacteria |
| Cell Wall Structure | Double-layered cell wall | Single-layered cell wall |
| Peptidoglycan Layer | Thin layer (1-3nm) | Thick layer (20-80nm) |
| Staining | Pink or red | Purple or blue |
| Lipopolysaccharides (LPS) | Present in outer membrane | Absent |
Figure 2: Differences Between Gram-Negative and Gram-Positive Bacteria
How Does Gram-Negative Bacteria Cause Disease?
Endotoxins
Gram-negative bacteria produce endotoxins, which are lipopolysaccharides (LPS) found in their outer cell membrane. These endotoxins can trigger a severe immune response in the host, leading to the release of pro-inflammatory cytokines, vascular leakage, and tissue damage. Conditions such as sepsis, a life-threatening systemic infection, can occur due to the release of endotoxins.
Virulence Factors
Virulence Factors: Gram-negative bacteria possess various virulence factors that aid in their survival and pathogenesis. These factors include adhesins, toxins, capsules, fimbriae, and efflux pumps. Adhesins allow the bacteria to attach to host tissues, toxins disrupt host cell function, capsules protect bacteria from the immune system, fimbriae assist in adhesion and colonization, and efflux pumps aid in antibiotic resistance.
Antibiotic Resistance
Antibiotic Resistance: Gram-negative bacteria have shown remarkable adaptability to antibiotics. Their unique cell wall structure, combined with the production of efflux pumps and enzymes that inactivate antibiotics, contributes to their resistance. This resistance poses a significant challenge in treating infections caused by Gram-negative bacteria, leading to increased morbidity and mortality rates.
Diseases Caused by Gram-Negative Bacteria and Associated Symptoms
Urinary Tract Infections (UTIs)
Gram-negative bacteria, particularly E. coli, are a common cause of UTIs. They can ascend the urinary tract and colonize the bladder, leading to symptoms such as frequent urination, pain, and fever.
Gastrointestinal Infections
Several Gram-negative bacteria, including Salmonella and Shigella species, are responsible for gastrointestinal infections. These bacteria can contaminate food and water sources, leading to food poisoning. Gram-negative food poisoning occurs when individuals consume food or water contaminated with these bacteria or their toxins. Salmonella is a common cause of gram-negative food poisoning. It is often associated with contaminated poultry, eggs, meat, and dairy products. Food poisoning can lead to symptoms such as diarrhea, abdominal pain, and vomiting.
Pneumonia
Gram-negative bacteria, such as Pseudomonas aeruginosa and Klebsiella pneumoniae, can cause severe pneumonia, especially in hospitalized or immunocompromised individuals. These infections can be life-threatening, requiring prompt and targeted antibiotic therapy. Effective prevention strategies in healthcare settings include implementing strict infection control measures, such as proper disinfection of surfaces and medical equipment, and adhering to strict hand hygiene protocols. Timely identification and isolation of patients with suspected Gram-negative pneumonia can also help minimize the spread of these pathogens within healthcare facilities. Furthermore, vaccination against common Gram-negative bacteria, such as Klebsiella pneumoniae, can provide an additional layer of protection for vulnerable individuals, reducing the risk of severe pneumonia.
Hospital-Acquired Infections
Gram-negative bacteria are a significant cause of healthcare-associated infections, often due to their multidrug resistance. These infections can occur in surgical sites, bloodstream (sepsis), urinary tract, and respiratory tract, leading to increased hospital stays, treatment costs, and patient mortality. The prevention of these infections requires a comprehensive approach that includes strict adherence to infection control protocols, such as proper sterilization of medical instruments and equipment, as well as meticulous hand hygiene practices by healthcare workers. Implementing antimicrobial stewardship programs is crucial to minimize the inappropriate use of antibiotics and reduce the development of multidrug-resistant Gram-negative strains.
Treatment of Gram-Negative Bacteria Infections
Antibiotics are the primary mode of treatment for Gram-negative bacterial infections. However, due to the unique structure of Gram-negative bacteria, certain considerations need to be taken into account. Antibiotics that can effectively penetrate the outer membrane are used. These medications typically utilize specific mechanisms to cross the outer membrane, such as utilizing porins, the small channels present in the outer membrane of Gram-negative bacteria. Once inside the bacterial cell, the antibiotics can target and inhibit essential cellular processes.
One class of antibiotics commonly used to treat Gram-negative infections is those containing a beta-lactam ring. These include antibiotics such as amoxicillin. Beta-lactam antibiotics work by interfering with the synthesis of the bacterial cell wall, ultimately leading to bacterial cell death. Another effective antibiotic for Gram-negative infections is ciprofloxacin. Ciprofloxacin belongs to the fluoroquinolone class of antibiotics and works by inhibiting the activity of enzymes that Gram-negative bacterial cells require for replication.
It is crucial to complete the full course of antibiotics as prescribed by a healthcare professional, even if the symptoms of infection start to improve. This ensures that all the bacteria are eradicated and helps prevent the development of antibiotic resistance.
Prevention of Gram Negative Infections
Prevention of Gram-negative infections is crucial in maintaining public health and reducing the risk of serious illnesses. Several key practices play a vital role in mitigating the spread of these infections. Regular handwashing is paramount, as it effectively eliminates harmful bacteria present on our hands. Additionally, proper wound care is essential to prevent the entry of Gram-negative bacteria into the body. Adopting a balanced diet strengthens the immune system, enabling the body to fight off potential infections more effectively. Good oral hygiene not only safeguards against oral infections but also reduces the risk of Gram-negative bacteria entering the bloodstream. Furthermore, safe food handling practices, such as proper cooking and storage, prevent contamination and the transmission of these pathogens. By incorporating these practices into our daily routines, we can significantly reduce the incidence of Gram-negative infections and safeguard our well-being.
Related Kits
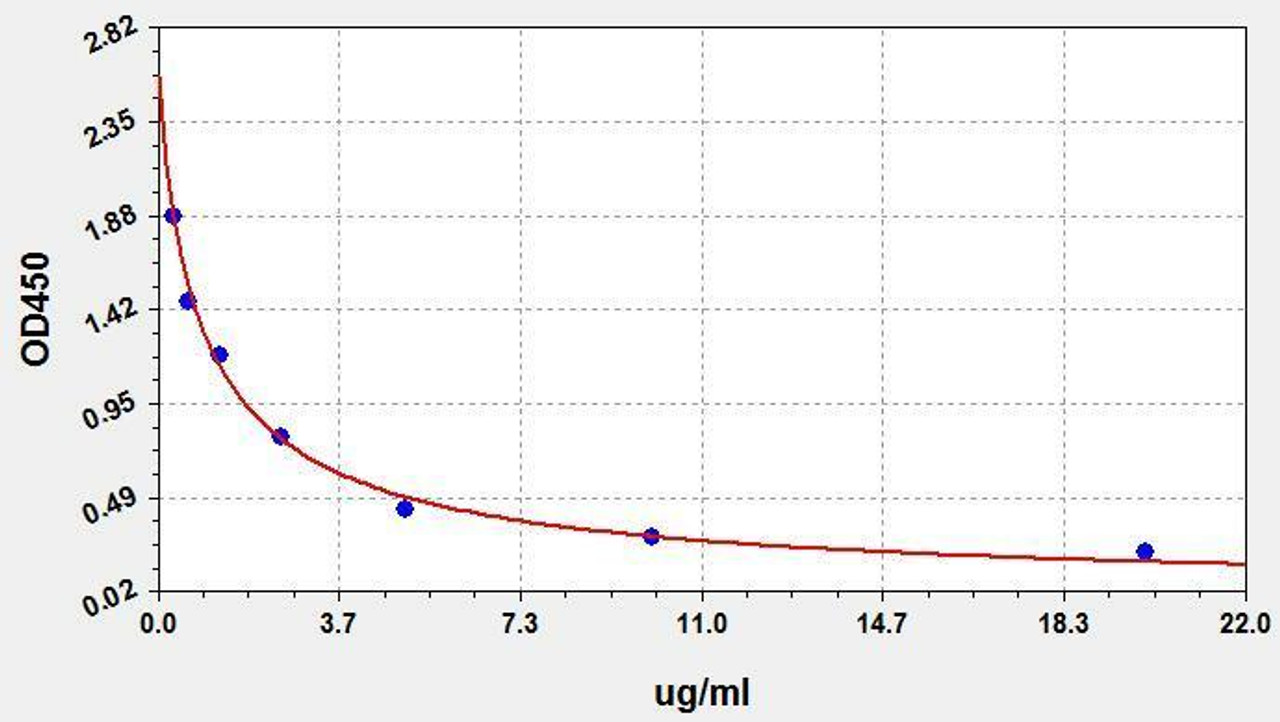
| LPS (Lipopolysaccharides) ELISA Kit | |
|---|---|
| ELISA Type | Competitive |
| Sensitivity | 0.188ug/ml |
| Range | 0.313-20ug/ml |
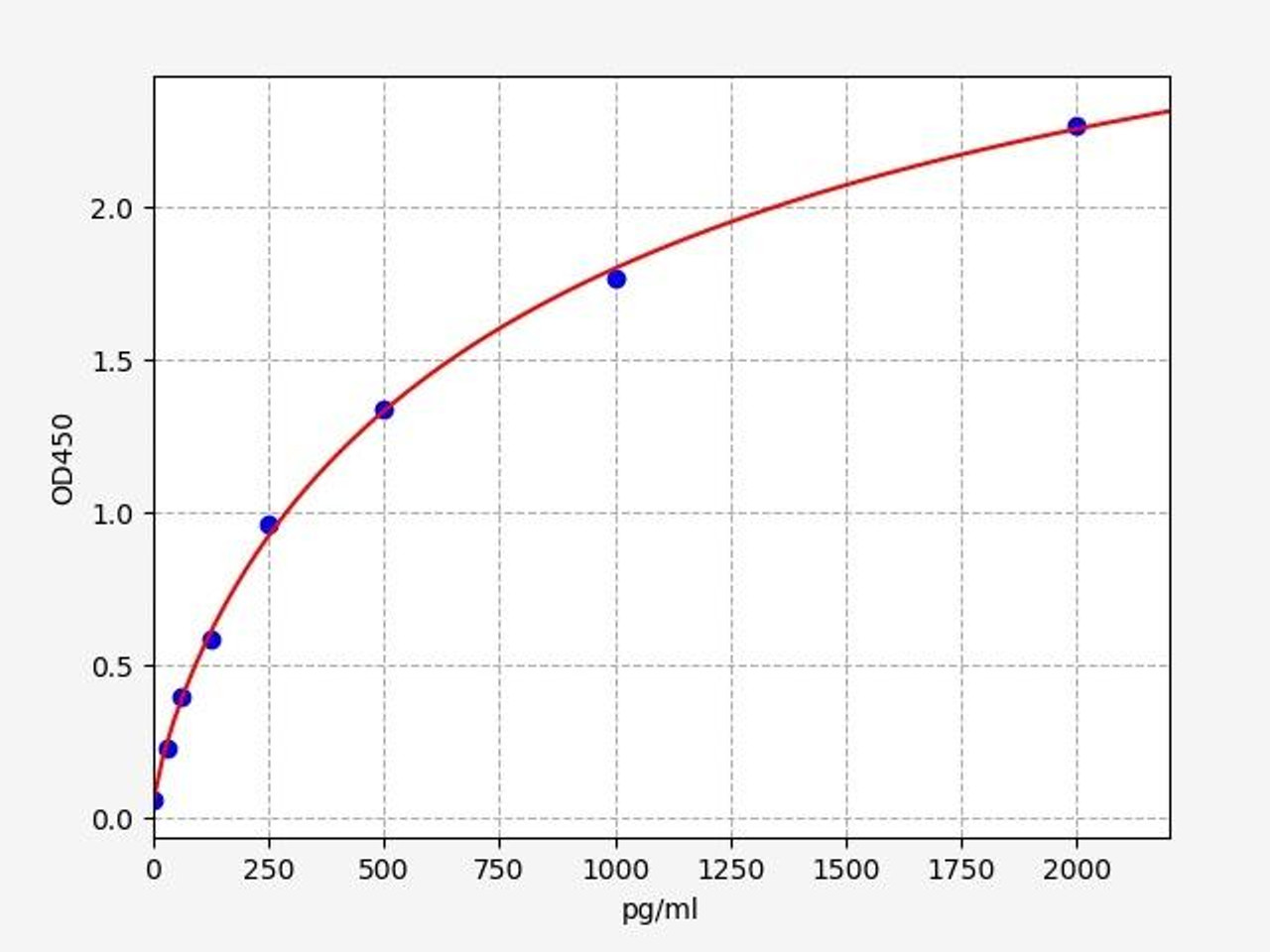
| Human IL-12 (p40) ELISA Kit | |
|---|---|
| ELISA Type | Sandwich |
| Sensitivity | 18.75pg/ml |
| Range | 31.25-2000pg/ml |
Written by Lauryn McLoughlin
Lauryn McLoughlin completed her undergraduate degree in Neuroscience before completing her masters in Biotechnology at University College Dublin.
Recent Posts
-
Enavatuzumab: Revolutionizing Cancer Research Through Novel Therapeutics
Quick Facts About EnavatuzumabWhat is Enavatuzumab?Enavatuzumab is a monoclonal antibo …17th Dec 2025 -
Alemtuzumab: Mechanism, Applications, and Biosimilar Advancements
Quick Facts About AlemtuzumabWhat is Alemtuzumab?Alemtuzumab is a monoclonal antibody …17th Dec 2025 -
Erenumab: Transforming Migraine Prevention Through CGRP Receptor Inhibition
Quick Facts About ErenumabWhat is Erenumab?Erenumab is a fully human monoclonal antibo …1st Apr 2025




