Non-Small Cell Lung Carcinoma: Understanding, Diagnosing, and Treating NSCLC
Non-Small Cell Lung Carcinoma (NSCLC) is the most common type of lung cancer, representing about 85% of all lung cancer cases. NSCLC includes several subtypes, with distinct biological characteristics that influence treatment options and prognosis. Advances in targeted therapies and immunotherapies have significantly improved NSCLC treatment, especially in advanced stages.
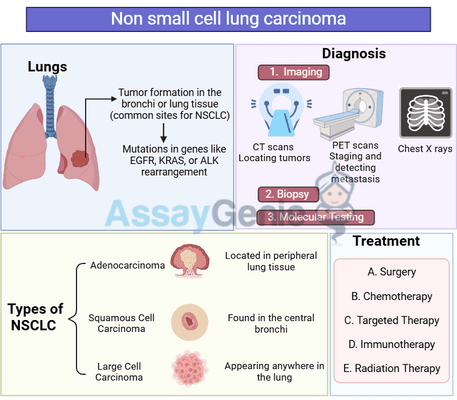
1. What is Non-Small Cell Lung Carcinoma?
NSCLC encompasses a group of lung cancers that arise from different types of lung cells and grow at varying rates. Unlike small cell lung carcinoma (SCLC), which is more aggressive, NSCLC generally progresses more slowly. The main types of NSCLC are:
- Adenocarcinoma: The most common subtype, often found in the outer areas of the lung, and
is associated with non-smokers as well as smokers. - Squamous Cell Carcinoma: Typically located in the central part of the lung, linked strongly with smoking.
- Large Cell Carcinoma: A less common, aggressive subtype that can occur in any part of the lung.
2. Risk Factors for NSCLC
Certain lifestyle, genetic, and environmental factors increase the risk of developing NSCLC:
- Smoking: The primary risk factor, with 80-90% of lung cancers linked to smoking or secondhand smoke.
- Radon Exposure: A radioactive gas that can accumulate indoors and is the second leading cause of lung cancer.
- Air Pollution: Long-term exposure to polluted air, including diesel exhaust and industrial emissions, increases risk.
- Occupational Hazards: Exposure to asbestos, arsenic, and other carcinogens in workplaces increases NSCLC risk.
- Family History and Genetics: Genetic predisposition can also play a role, especially in non-smokers who develop lung cancer.
3. Symptoms of NSCLC
Symptoms of NSCLC can vary depending on the cancer’s location, size, and stage. Early NSCLC is often asymptomatic, with symptoms appearing as the tumor grows.
Common Symptoms
- Persistent Cough: A new cough that does not go away or changes in a smoker’s cough.
- Hemoptysis: Coughing up blood or bloody mucus.
- Chest Pain: Pain in the chest that worsens with deep breathing, coughing, or laughing.
- Shortness of Breath: Due to airway obstruction or pleural effusion.
- Unexplained Weight Loss: Often accompanied by loss of appetite.
- Hoarseness: Caused by tumor pressure on nerves in the chest.
Early detection is crucial for effective treatment, so any persistent respiratory symptoms should be evaluated.
4. Diagnosis of NSCLC
Imaging Tests
- Chest X-Ray: Initial imaging for any respiratory symptoms, though limited in detail.
- CT Scan: Provides detailed cross-sectional images of the lungs, often used to confirm suspicious findings from an X-ray.
- PET Scan: Helps detect metastasis by showing areas of high metabolic activity.
- MRI: Used to assess brain metastases, especially in advanced NSCLC.
Biopsy and Molecular Testing
- Bronchoscopy: A tube with a camera is passed through the airway to collect tissue samples.
- Needle Biopsy: Tissue is sampled with a needle, often guided by CT imaging.
- Surgical Biopsy: Sometimes necessary to obtain larger tissue samples.
Molecular testing for mutations like EGFR, ALK, ROS1, and PD-L1 expression guides treatment choices, particularly for targeted and immunotherapies.
5. Staging of NSCLC
Staging NSCLC is essential for determining the treatment approach and prognosis. NSCLC is staged using the TNM system:
- Stage I: Tumor confined to the lung, with no lymph node involvement.
- Stage II: Tumor spread to nearby lymph nodes or other nearby structures.
- Stage III: Tumor spread to lymph nodes in the middle of the chest or other nearby structures.
- Stage IV: Metastasis to distant organs, such as the liver, brain, bones, or adrenal glands.
6. Treatment Options for NSCLC
Treatment options for NSCLC vary by stage and genetic profile, with curative options focused on early stages and palliative approaches for advanced stages.
Surgery
Surgery is a primary treatment for early-stage NSCLC, aiming to remove the tumor.
- Lobectomy: Removal of a lobe of the lung, the standard treatment for resectable NSCLC.
- Pneumonectomy: Removal of an entire lung, used for larger tumors.
- Segmentectomy or Wedge Resection: Partial lung removal, typically for small, localized tumors or patients with limited lung function.
Radiation Therapy
Radiation therapy is often used for patients who are not candidates for surgery or to control symptoms in advanced NSCLC.
- Stereotactic Body Radiotherapy (SBRT): Highly targeted radiation for small tumors.
- External Beam Radiation Therapy (EBRT): For larger tumors or metastases.
- Adjuvant Radiation: Used post-surgery to eliminate remaining cancer cells.
Chemotherapy
Chemotherapy may be used alone or with other therapies in more advanced stages:
- Neoadjuvant Chemotherapy: Given before surgery to shrink tumors.
- Adjuvant Chemotherapy: Given post-surgery to target any remaining cancer cells.
- Palliative Chemotherapy: To relieve symptoms in advanced NSCLC.
Common agents include cisplatin, carboplatin, paclitaxel, and pemetrexed.
Targeted Therapy
Targeted therapy is based on specific genetic mutations in the cancer cells:
- EGFR Inhibitors: Drugs like erlotinib and osimertinib target EGFR mutations.
- ALK Inhibitors: Alectinib and crizotinib target ALK-positive NSCLC.
- ROS1 and BRAF Inhibitors: Used for tumors with ROS1 or BRAF mutations, as determined by genetic testing.
Immunotherapy
Immunotherapy has become a breakthrough treatment for NSCLC, particularly for advanced and metastatic stages.
- Checkpoint Inhibitors: Pembrolizumab (anti-PD-1) and nivolumab enhance the immune system's ability to recognize and destroy cancer cells.
- Combination Therapy: Checkpoint inhibitors are often combined with chemotherapy or targeted therapies for enhanced effectiveness.
Clinical Trials
Clinical trials for NSCLC continue to explore novel therapies, including new immunotherapies, combination regimens, and CAR T-cell therapies targeting lung cancer antigens.
7. Prognosis and Survival Rates
The prognosis for NSCLC varies based on the stage at diagnosis and treatment response.
- Localized NSCLC (Stages I-II): The 5-year survival rate is relatively high, around 60-70% with treatment.
- Regional NSCLC (Stage III): The survival rate decreases, generally ranging from 20-40%.
8. Advances in NSCLC Research
Liquid Biopsies
Liquid biopsies, which analyze circulating tumor DNA (ctDNA) in the blood, offer a non-invasive approach for detecting mutations and monitoring treatment response in NSCLC, especially for patients with metastatic disease.
Personalized Therapy
Advances in genetic testing allow for personalized treatment based on specific mutations, improving treatment efficacy and minimizing unnecessary side effects.
CAR T-Cell Therapy
Although traditionally used in blood cancers, CAR T-cell therapy is being investigated for NSCLC, focusing on engineering T cells to target specific lung cancer antigens.
Conclusion
Non-small cell lung carcinoma remains a challenging diagnosis, but recent advances in targeted therapies, immunotherapies, and personalized treatment have opened up new possibilities. Early detection remains key for improving survival, and ongoing research continues to provide hope for better treatments and outcomes for NSCLC patients.
Recent Posts
-
Enavatuzumab: Revolutionizing Cancer Research Through Novel Therapeutics
Quick Facts About EnavatuzumabWhat is Enavatuzumab?Enavatuzumab is a monoclonal antibo …17th Dec 2025 -
Alemtuzumab: Mechanism, Applications, and Biosimilar Advancements
Quick Facts About AlemtuzumabWhat is Alemtuzumab?Alemtuzumab is a monoclonal antibody …17th Dec 2025 -
Validation of MycoGenie Rapid Mycoplasma Detection Kit - A highly sensitive visual determination method for Mycoplasma detection.
The MycoGenie Rapid Mycoplasma Detection Kit enables the detection of 28 Mycoplasma sp …3rd Mar 2025