von Willebrand Factor and Cancer
What is von Willebrand Factor?
Von Willebrand Factor (VWF) is a crucial glycoprotein that plays a fundamental role in blood clotting and hemostasis. Produced by endothelial cells and megakaryocytes, VWF circulates in the bloodstream as large multimers. Its primary function is to mediate platelet adhesion at sites of vascular injury, forming a temporary platelet plug to stop bleeding. VWF also serves as a carrier protein for Factor VIII, protecting it and extending its availability during the clotting process.
Von Willebrand Disease (VWD) is an inherited bleeding disorder caused by deficiencies or abnormalities in von Willebrand Factor.
Structure and Function of von Willebrand Factor
VWF is a large multimeric protein composed of repeating units known as monomers, which are linked together to form different sizes of multimers, ranging from small dimers to extremely large forms containing thousands of monomers. Importantly, VWF is secreted by EC in a highly multimeric string-like form known as Ultra-Large VWF (UL-VWF). The multimeric composition of VWF is a key determinant of its activity. VWF strings can unwind via circulatory stresses, exposing further binding sites along the structure, including platelet binding site GPIbα, P-selectin, and collagen. This allows VWF to serve as a versatile adhesive molecule, promoting platelet adhesion and aggregation under high shear stress conditions in the blood vessels. However, these UL-VWF strings are broken down by a VWF-cleaving protease A Disintegrin And Metalloproteinase with Thrombospondin Type 1 Motif, 13 (ADAMTS13), resulting in the production of less biologically active multimers known as low molecular weight multimers (LMWM) before being cleared from the circulation. The VWF gene, located on chromosome 12, encodes the precursor protein pre-pro-VWF, which undergoes several post-translational modifications to become mature VWF. After signal peptide cleavage and glycosylation, VWF forms pro-VWF, which further undergoes proteolytic processing in the endoplasmic reticulum and Golgi apparatus to generate the mature VWF multimers.
VWF consists of several functional domains, each serving specific roles in its biological functions. Notably, the A1 domain is responsible for mediating adhesion between VWF and platelets, facilitating platelet aggregation at the site of vessel injury. The A2 domain is crucial for interacting with subendothelial collagen, contributing to VWF's anchoring to the injured vessel wall. The A3 domain plays a role in self-association, leading to the formation of large multimers that are essential for effective clot formation. The complex and dynamic structure of VWF allows it to act as a versatile adhesive molecule, promoting platelet adhesion and aggregation under high shear stress conditions in the blood vessels.
Moreover, VWF serves as a carrier protein for Factor VIII, protecting it from rapid degradation and extending its lifespan in the bloodstream. This stabilized Factor VIII is then released to participate in the coagulation cascade, ensuring effective clot formation.
Schematic of von Willebrand Factor
von Willebrand Factor (VWF) and Cancer
Von Willebrand Factor (VWF) exhibits a multifaceted role in cancer biology, impacting cancer-associated coagulopathies, tumor progression, angiogenesis, metastasis, and its potential as a biomarker.
VWF and Angiogenesis in Cancer
Angiogenesis, the process of forming new blood vessels from pre-existing ones, is a hallmark of cancer development and metastasis. In this context, VWF has emerged as a key player in regulating angiogenesis within the tumor microenvironment. Research has revealed that VWF contributes to tumor angiogenesis through its interactions with endothelial cells and pro-angiogenic factors. By engaging with specific receptors on endothelial cells, VWF triggers signaling cascades that promote endothelial cell migration and proliferation. This process, in turn, facilitates the angiogenic response, promoting neovascularization and the development of a dense vascular network to support the expanding tumor volume with vital nutrients and oxygen. Moreover, VWF's association with pro-angiogenic factors amplifies the neovascularization process, ensuring a well-organized vascular network within the tumor. The pro-angiogenic effects of VWF offer a potential target for anti-cancer therapies. Disrupting VWF-mediated angiogenesis has shown promise in preclinical studies as a strategy to inhibit tumor growth and metastasis. Developing therapies that specifically target VWF interactions in the tumor microenvironment may hold therapeutic potential for certain cancer types.
VWF and Metastasis
Metastasis, the spread of cancer cells from the primary tumor to distant organs, remains a significant challenge in cancer treatment. Recent investigations have highlighted VWF's role in facilitating cancer cell metastasis, shedding light on its potential impact on disease progression. VWF promotes metastasis by aiding cancer cell adhesion and invasion into the vascular endothelium. By interacting with integrins and other adhesion molecules expressed on cancer cells, VWF facilitates their attachment to the blood vessel walls and subsequent extravasation into surrounding tissues. This critical step allows cancer cells to disseminate through the bloodstream to establish secondary tumors in distant organs.
VWF and Microthrombi Formation
Elevated levels of VWF have been observed in various cancer types, and this increase in VWF concentration can contribute to the formation of microthrombi - small blood clots that develop in the tumor microvasculature. The formation of microthrombi within the tumor bears a two-sided impact. On one hand, it may help control bleeding and limit tumor expansion by obstructing blood flow to the tumor. However, on the other hand, microthrombi can create a pro-coagulant environment that promotes tumor progression. Microthrombi have been shown to facilitate the survival and proliferation of cancer cells by providing a protective shield against immune surveillance. They can also contribute to hypoxia and nutrient deprivation within the tumor, leading to the selection of more aggressive cancer cell populations. Additionally, microthrombi may hinder the delivery and efficacy of cancer treatments by impeding drug penetration into the tumor mass.
VWF and Coagulopathies
Von Willebrand Factor plays a crucial role in cancer-associated coagulopathies, presenting a significant clinical challenge for cancer patients. Thrombosis, particularly venous thromboembolism (VTE), is a common complication observed in up to 20% of cancer patients, leading to increased mortality rates. The tumor microenvironment can trigger a pro-coagulant state characterized by elevated VWF levels, promoting platelet activation and microthrombi formation within the tumor vasculature. These microthrombi contribute to tumor progression and metastasis, while also posing a risk of embolizatioan to distant organs.
In the pursuit of targeted therapies, researchers are exploring strategies to modulate VWF function, including VWF inhibitors and agents that interfere with VWF-mediated platelet activation. These interventions aim to disrupt the pro-coagulant effects of VWF and alleviate thrombotic complications in cancer patients.
VWF Related Kits
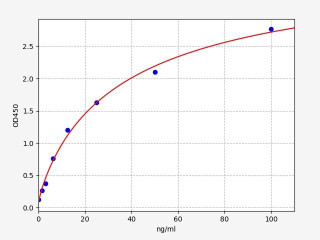
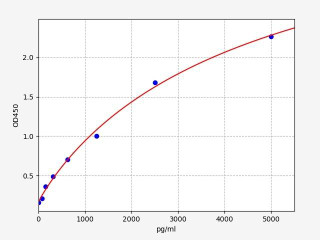
| Human VWF (Von Willebrand Factor) ELISA Kit | |
|---|---|
| ELISA Type | Sandwich |
| Sensitivity | 0.938ng/ml |
| Range | 1.563-100ng/ml |
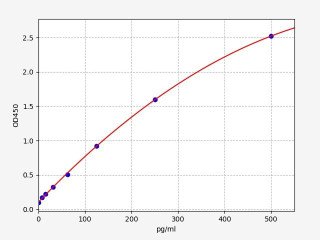
| Human Tissue factor / Coagulation Factor III ELISA Kit | |
|---|---|
| ELISA Type | Sandwich |
| Sensitivity | 4.688pg/ml |
| Range | 7.813-500pg/ml |
VWF and Serum Levels
There is now evidence to support a relationship between tumur size, metastasis and mortality with rising VWF serum levels. The data suggests that tumour cells can fine-tune the production of VWF through both EC activation and de novo VWF biosynthesis. Harmonious upregulation of VWF serum levels in the tumour microenvironment help to conduct the multi-faceted tumour promoting functions of VWF. These effects include potentially driving a self-proliferative inflammatory cycle, regulating angiogenesis in tumours and finally, promoting metastasis to distant sites. However, this effect can strike the wrong note and produce excessive VWF within the circulation culminating in a buildup of VWF, which can cause fatal thrombotic complications like VTE and TTP.
Written by Lauryn McLoughlin
Lauryn McLoughlin completed her undergraduate degree in Neuroscience before completing her masters in Biotechnology at University College Dublin.
Recent Posts
-
Enavatuzumab: Revolutionizing Cancer Research Through Novel Therapeutics
Quick Facts About EnavatuzumabWhat is Enavatuzumab?Enavatuzumab is a monoclonal antibo …17th Dec 2025 -
Alemtuzumab: Mechanism, Applications, and Biosimilar Advancements
Quick Facts About AlemtuzumabWhat is Alemtuzumab?Alemtuzumab is a monoclonal antibody …17th Dec 2025 -
Validation of MycoGenie Rapid Mycoplasma Detection Kit - A highly sensitive visual determination method for Mycoplasma detection.
The MycoGenie Rapid Mycoplasma Detection Kit enables the detection of 28 Mycoplasma sp …3rd Mar 2025