Understanding the Gut-Brain Axis
The gut-brain axis, a dynamic bi-directional communication system linking the gastrointestinal (GI) tract with the central nervous system (CNS), has emerged as a focal point in scientific research. This intricate network underscores the interconnectedness of physiological processes, revealing how the gut microbiota interfaces with cognitive functions. Beyond its conventional digestive role, the gut plays a pivotal role in shaping neurological processes, emotions, and behavior. Through neural pathways, hormonal signaling, and immune mediators, the gut and brain engage in a continuous dialogue, unraveling a previously unexplored dimension of human physiology and its potential implications for health and disease.
Table of Contents
Jump to a section:
What is the Gut-Brain Axis?
The Gut-Brain axis is a sophisticated bidirectional communication network that connects the central nervous system (CNS), encompassing the brain and spinal cord, with the enteric nervous system (ENS), located within the gastrointestinal tract. This intricate connection enables constant information exchange between the gut and the brain, encompassing neural pathways, hormonal signaling, and immune interactions. Moreover, the gut microbiota, a complex community of microorganisms residing in the gut, plays a vital role in this axis by influencing and being influenced by both the CNS and ENS. This dynamic interplay has far-reaching implications, impacting not only digestive processes but also cognitive functions, emotions, and overall health.
Fig. 1: An overview of the Gut Brain Axis, the components and clinical implications
Brain-Gut Connection - Components
The complex interaction of the gut-brain axis is influenced by various essential components that work together to establish communication between the gut and the brain. These components include the immune system, neuro-endocrine system, enteric nervous system, circulatory system, and a notable player, the vagus nerve. Another critical aspect we'll delve into is the gut microbiome—a collection of microorganisms in the gut that has a significant impact on this axis. Together, these elements orchestrate the flow of information between our gut and brain, shaping our overall well-being and health.
Immune System
The immune system serves as a sentinel, safeguarding against pathogens and regulating inflammation. Within the gut-brain axis, immune cells and molecules traverse the bloodstream, carrying information between the gut and the brain. Immune responses triggered by factors such as diet, stress, and gut dysbiosis can influence both local gut functions and distant brain processes, contributing to the axis's dynamic equilibrium.
Neuro-Endocrine System:
The neuro-endocrine system acts as a bridge between the nervous and endocrine systems, releasing hormones that modulate physiological processes. In the context of the gut-brain axis, hormones such as cortisol and serotonin play vital roles. Cortisol, released during stress, can impact gut functions and microbial balance. Serotonin, a neurotransmitter known for its role in mood regulation, is also abundant in the gut, where it influences gastrointestinal motility and gut-brain communication.
Enteric Nervous System (ENS):
The enteric nervous system, often termed the "second brain," resides within the gut walls. Comprising an intricate network of neurons, the ENS governs gut functions independently, coordinating processes like peristalsis and enzyme secretion. Through its neural pathways, the ENS communicates bidirectionally with the central nervous system, forming a fundamental component of the gut-brain axis.
Circulatory System:
The circulatory system, encompassing blood vessels and the cardiovascular system, is crucial for transporting nutrients, oxygen, and signaling molecules. In the context of the gut-brain axis, blood vessels facilitate the exchange of metabolites and bioactive compounds between the gut and the brain. These compounds include neurotransmitters, hormones, and immune mediators that contribute to the regulatory conversations within the axis.
Vagus Nerve:
The vagus nerve, an integral part of the autonomic nervous system, serves as a vital conduit for gut-brain communication. It carries sensory information from the gut to the brain and enables the brain to influence gut functions. Through the release of neurotransmitters like acetylcholine, the vagus nerve modulates various physiological responses, further underscoring its role as a central player in the gut-brain axis.
Intestinal Flora (Microbiome)
Central to the gut-brain axis is the gut microbiome, an intricate assembly of microorganisms that inhabit the gastrointestinal tract. These microbes engage in a dynamic cross-talk with the nervous and immune systems, releasing metabolites and bioactive compounds that influence brain function and behavior. The gut microbiome's impact on the axis underscores its significance in shaping both gut health and cognitive processes.
Fig 2: An overview of Microbiome Sign
Gut-Brain Axis Pathway Secretions
The intricate communication within the gut-brain axis is facilitated by a multitude of secretions, including neurotransmitters, hormones, and bioactive compounds. These secretions serve as messengers that convey information between the gastrointestinal tract and the central nervous system, influencing various physiological and cognitive processes.
Neurotransmitters in the Gut
Neurotransmitters are chemicals that transmit signals between nerve cells. Within the gut-brain axis, neurotransmitters like serotonin, dopamine, and gamma-aminobutyric acid (GABA) play essential roles. Serotonin, found abundantly in the gut, contributes to mood regulation, gastrointestinal motility, and the perception of pain. Dopamine impacts reward and pleasure responses, affecting gut motility and function. GABA, known for its calming effects, influences gut movements and responses to stress.
Hormones
Hormones are chemical messengers produced by various glands in the body. In the context of the gut-brain axis, hormones like cortisol, insulin, and ghrelin contribute to the intricate communication between the gut and the brain. Cortisol, released during stress, influences gut motility, immune responses, and microbial balance. Insulin, which regulates blood sugar, can impact appetite and gut functions. Ghrelin, often referred to as the "hunger hormone," signals hunger to the brain, influencing eating behavior.
Bioactive Compounds
Bioactive compounds, including short-chain fatty acids (SCFAs) produced by gut microbiota, have gained prominence for their role in the gut-brain axis. SCFAs serve as energy sources for gut cells and impact immune responses. Additionally, they can cross the blood-brain barrier, influencing brain function and cognitive processes. By interacting with receptors on nerve cells and immune cells, SCFAs contribute to the complex interplay between the gut and the brain.
Enteric Hormones
The gut also produces hormones known as enteric hormones, which regulate various aspects of digestion and gut functions. For example, cholecystokinin (CCK) is released in response to food intake and impacts digestion and satiety. Gastrin influences stomach acid production and motility. These enteric hormones not only govern local gut processes but also communicate with the brain, shaping overall digestive and physiological responses.
ELISA Kits Related to the Gut-Brain Axis
ELISA Kits
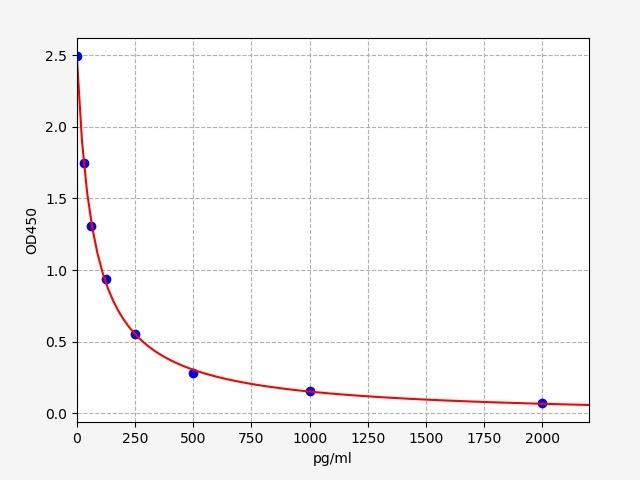
| Human CCK (Cholecystokinin) ELISA Kit | |
|---|---|
| ELISA Type: | Competitive |
| Sensitivity: | 9.375pg/ml |
| Range: | 15.625-1000pg/ml |

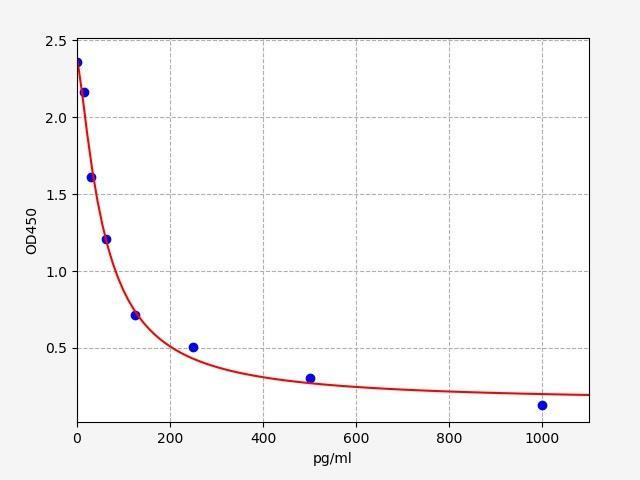
| Cortisol (Cortisol) ELISA Kit | |
|---|---|
| ELISA Type: | Competitive |
| Range: | 0.78-50 ng/mL |
| Reactivity: | Universal |
Factors that Influence the Gut-Brain Axis
The equilibrium of the gut-brain axis is subject to the influence of various pivotal factors, underscoring the delicate interplay between the gut and the brain. Dietary choices wield a substantial impact, as diets rich in fiber and diverse plant-based foods promote a thriving gut microbiota, which in turn affects cognitive function. Conversely, diets high in processed foods and sugars may disrupt this balance, potentially affecting mood and cognitive processes. Stress emerges as a potent modulator, triggering physiological changes in the gut and influencing mental well-being. Chronic stress can disrupt the axis, potentially exacerbating conditions like irritable bowel syndrome (IBS) and mental health disorders.
Gut Microbiome Composition
Microbiota composition constitutes another key factor, its balance shaped by diet, antibiotics, and environmental exposures. Dysbiosis, an imbalance in gut microbes, can perturb the gut-brain axis, potentially contributing to mood disorders and cognitive impairments. Antibiotics and certain medications, while necessary, can also impact the axis by affecting gut microbial composition. Environmental factors and lifestyle choices, including exposure to pollutants, physical activity, and sleep patterns, further interact with the gut-brain axis. By understanding and addressing these multifaceted factors, we can aspire to cultivate a resilient gut-brain axis, fostering holistic well-being that spans both the physiological and cognitive domains.
Dysregulation of the Gut-Brain Axis
The disruption of the gut-brain axis, termed dysregulation, can have profound implications for both neurodevelopment and neuropsychiatric conditions as well as neurodegenerative disorders.
Neurodegenerative Disorders
Dysregulation of the gut-brain axis also has implications for neurodegenerative disorders such as Parkinson's disease and Alzheimer's disease. Accumulating evidence suggests that alterations in gut microbiota composition may precede the onset of these disorders. In Parkinson's disease, for instance, changes in gut microbial populations are associated with motor and non-motor symptoms. Dysbiosis in the gut-brain axis may contribute to neuroinflammation and protein aggregation, hallmarks of neurodegenerative diseases.
Furthermore, the gut-brain axis's disruption can impact the blood-brain barrier, which normally acts as a protective barrier between the brain and circulating substances. A compromised blood-brain barrier allows substances from the gut to enter the brain, potentially exacerbating neuroinflammation and cognitive decline in neurodegenerative conditions.
Neurodevelopmental Conditions
Dysregulation of the gut-brain axis has been implicated in neurodevelopmental and neuropsychiatric conditions such as autism spectrum disorder (ASD) and mood disorders. Perturbations in gut microbiota composition and function have been observed in individuals with ASD, suggesting a link between microbial imbalances and neurological development. The axis's dysregulation in these conditions may contribute to altered neurotransmitter levels, immune responses, and inflammation, potentially influencing behaviors and cognitive functions.
Gut Microbiome and Mental Health
In neuropsychiatric disorders like depression and anxiety, disruptions in the gut-brain axis have garnered attention. Changes in gut microbial diversity and the subsequent effects on neurotransmitter metabolism can influence mood regulation. Emerging research explores interventions targeting the gut microbiota as a potential avenue for ameliorating symptoms and improving mental well-being.
Conclusion
Our journey through the intricate world of the gut-brain axis reveals how our body and mind are closely linked. The different parts—like the gut's nervous system, hormones, and gut bugs—all work together to send messages between our gut and brain. We've seen how what we eat, how we handle stress, and even the tiny creatures living in our gut can impact this connection.
By understanding this axis, we gain insights into why things like autism, mood troubles, and memory problems might happen. These issues show us how important the gut-brain connection is for our health. Even though there's a lot more to learn, we're moving forward in finding ways to help people using this knowledge.
The gut-brain axis isn't just a scientific discovery; it's a path to better health and happiness. As we explore and learn more, we open doors to new ways of helping people lead healthier lives by keeping both their gut and brain in balance.
Written by Rithika Suresh
Rithika Suresh completed her undergraduate degree in Biotechnology in Anna University before completing her masters in Biotechnology at University College Dublin.
Recent Posts
-
Enavatuzumab: Revolutionizing Cancer Research Through Novel Therapeutics
Quick Facts About EnavatuzumabWhat is Enavatuzumab?Enavatuzumab is a monoclonal antibo …17th Dec 2025 -
Alemtuzumab: Mechanism, Applications, and Biosimilar Advancements
Quick Facts About AlemtuzumabWhat is Alemtuzumab?Alemtuzumab is a monoclonal antibody …17th Dec 2025 -
Validation of MycoGenie Rapid Mycoplasma Detection Kit - A highly sensitive visual determination method for Mycoplasma detection.
The MycoGenie Rapid Mycoplasma Detection Kit enables the detection of 28 Mycoplasma sp …3rd Mar 2025