Platelets : The Unassuming Heroes of Blood Circulation
Platelets, the tiny cellular fragments found in our blood, play a crucial role in maintaining our overall health and well-being. From their role in blood clotting to their involvement in immune responses, these tiny cells are essential players in the intricate symphony of our circulatory system. In this blog post, we will delve into the world of platelets, exploring their structure, function, and clinical significance. From their formation in the bone marrow to their use in medical treatments, we will uncover the remarkable contributions of platelets to our body's resilience and their impact on various health conditions.
Table of Contents
Jump to a section:
What are Platelets?
Platelets, also known as thrombocytes, are tiny, disc-shaped cellular components present in the blood of vertebrates, including humans. They are a crucial element of the circulatory system and play a vital role in maintaining hemostasis, the process that prevents excessive bleeding after an injury or damage to blood vessels. Platelets are produced in the bone marrow through a complex process called thrombopoiesis, which involves the differentiation and maturation of precursor cells.
How are platelets formed?
Platelets are formed through a process called thrombopoiesis, which takes place in the bone marrow. The main precursor cells involved in thrombopoiesis are called megakaryocytes. These large and unique bone marrow cells undergo a series of complex steps to produce platelets.
1. Megakaryocyte Development: Megakaryocytes originate from hematopoietic stem cells, which are unspecialized cells in the bone marrow responsible for producing all types of blood cells. Hematopoietic stem cells differentiate into specialized progenitor cells, including megakaryocyte-erythroid progenitors, which further develop into megakaryocyte lineage cells.
2. Maturation of Megakaryocytes: As megakaryocytes mature, they undergo a process called endomitosis, where their nucleus replicates multiple times without cell division, leading to an increase in DNA content. This unique characteristic allows megakaryocytes to become large and polyploid, containing multiple sets of chromosomes within a single cell.
3. Platelet Formation: Once the megakaryocytes reach maturity, they extend long protrusions called proplatelets into the blood vessels within the bone marrow. These proplatelets undergo a series of fission events, resulting in the formation of numerous platelets that are released into the bloodstream.
4. Regulation of Thrombopoiesis: Thrombopoiesis is tightly regulated to maintain appropriate platelet levels in the blood. Thrombopoietin, a hormone produced primarily in the liver and kidneys, plays a key role in stimulating the proliferation and maturation of megakaryocytes, thereby influencing platelet production.
Explore our Thrombopoietin Assays:
Fig 1. Thrombopoiesis Overview
Platelet Shape and Structure
Shape of Platelets
The typical shape of platelets is discoid, which means they resemble a biconvex lens or a small plate. This morphology allows them to have a larger surface area relative to their volume, facilitating efficient adhesion and aggregation at the site of injury. Additionally, their discoid shape aids in smooth flow through blood vessels, minimizing the risk of vessel occlusion while maximizing their responsiveness during hemostasis.
Despite their initial discoid form, platelets are highly dynamic cells capable of changing their shape dramatically upon activation. When a blood vessel is injured, platelets adhere to the exposed collagen fibers and undergo a process known as shape change or platelet activation. During this process, platelets extend numerous projections called pseudopodia, which allow them to interact with other platelets and components of the blood clotting cascade. This shape change is essential for the recruitment and aggregation of more platelets, forming a stable clot to prevent further blood loss.
Structure of Platelets
Platelets, as cellular components of the blood, have a complex structure that enables them to perform their essential functions in hemostasis and other physiological processes. While they lack a nucleus, platelets contain various specialized organelles and molecules within their cytoplasm, contributing to their unique capabilities. Inside a mature platelet, there are four distinct zones or regions.
1. Peripheral Zone: The peripheral zone is the outermost region of the platelet. It contains the plasma membrane, which is rich in glycoproteins and surface receptors. These glycoproteins play a crucial role in platelet adhesion and aggregation when the platelet encounters damaged blood vessel walls.
2. Sol-Gel Zone: The sol-gel zone lies just beneath the peripheral zone and contains a dense network of microtubules and microfilaments, primarily composed of actin and myosin. This region is responsible for platelet shape change, cytoskeletal rearrangement, and platelet contraction during clot retraction.
3. Organelle Zone: The organelle zone contains the platelet's internal organelles, including the granules. As mentioned earlier, platelets have two main types of granules: alpha granules and dense granules. The alpha granules contain proteins, clotting factors, and growth factors involved in clot formation and tissue repair. The dense granules store small molecules such as ADP and calcium, which are crucial for platelet activation and aggregation.
4. Membrane System: The membrane system or open canalicular system (OCS) is a network of open channels running through the platelet's interior. This system allows for rapid communication and exchange of ions, small molecules, and signaling molecules between the platelet cytoplasm and the surrounding plasma. The OCS is involved in amplifying platelet activation signals and coordinating the response to vascular injuries.
Platelet Function
Platelets, as vital components of the blood, serve a fundamental role in various physiological processes, primarily related to hemostasis, the body's mechanism to prevent and control bleeding after vascular injury. Additionally, platelets play essential roles beyond hemostasis, contributing to immune responses and tissue repair.
Platelets in blood clotting
Platelets play a central role in blood clotting, also known as coagulation, which is a complex process involving the formation of a stable blood clot to prevent excessive bleeding. When a blood vessel is injured, platelets are immediately activated, leading to a series of events that result in clot formation.
1. Adhesion: Upon vascular injury, platelets adhere to the exposed collagen fibers at the site of injury through specific surface receptors, primarily glycoprotein Ib-IX-V. This initial adhesion is crucial for platelet accumulation and the formation of a stable clot.
2. Activation: Adhesion triggers platelet activation, causing them to change shape and release the contents of their granules, such as ADP, calcium, and clotting factors. This release promotes further platelet aggregation and recruits additional platelets to the site of injury.
3. Aggregation: Activated platelets aggregate, forming a primary hemostatic plug or platelet plug. The glycoprotein IIb/IIIa receptors on the platelet surface bind to fibrinogen, linking adjacent platelets together and strengthening the platelet plug.
4. Clot Formation: The activated platelet plug serves as a scaffold for the deposition of fibrin, a protein that forms a mesh-like network to stabilize the clot further. This process is mediated by the coagulation cascade, involving a series of clotting factors and enzymes.
Are Platelets Part of the Immune System?
While platelets are primarily known for their role in hemostasis and blood clotting, emerging research has highlighted their involvement in immune responses. Platelets possess various immunomodulatory properties and interact with other immune cells, contributing to both inflammatory and immune defense processes.
1. Immune Cell Interaction: Platelets can interact with various immune cells, such as leukocytes, endothelial cells, and macrophages. These interactions facilitate the recruitment and activation of immune cells during inflammation and immune responses.
2. Cytokine Release: Activated platelets release cytokines and chemokines, which are signaling molecules that influence the behavior and function of other immune cells. This cytokine release can modulate immune responses, inflammation, and wound healing.
3. Pathogen Defense: Platelets can recognize and respond to pathogens directly, contributing to the immune defense against infections. They can interact with pathogens and activate defense mechanisms, acting as an essential link between hemostasis and immunity.
Platelet Activation
Platelet activation is a critical physiological process that occurs in response to vascular injury or other triggers. Upon activation, platelets change from their quiescent, discoid shape to an activated, more spherical form. This transformation is essential for initiating and amplifying the hemostatic response, leading to the formation of blood clots at the site of injury.
Mechanisms of Platelet Activation:
Platelet activation involves a series of intracellular signaling pathways and molecular events that lead to changes in platelet shape, granule release, and enhanced adhesiveness. Some key mechanisms of platelet activation include:
1. Platelet Surface Receptors: Platelets possess various surface receptors, including glycoprotein IIb/IIIa and glycoprotein Ib-IX-V, which play critical roles in platelet activation. When these receptors interact with specific ligands, such as fibrinogen or von Willebrand factor, it triggers a signaling cascade that leads to platelet aggregation and clot formation.
2. ADP and Thromboxane A2 (TxA2) Release: Upon activation, platelets release ADP and TxA2 from their dense granules. These molecules act as powerful platelet agonists, promoting further platelet activation and aggregation. ADP binds to specific receptors on platelets, leading to shape change and granule release, while TxA2 promotes vasoconstriction and enhances platelet aggregation.
3. Calcium Influx: Activation induces an increase in intracellular calcium levels in platelets, which is essential for their shape change, granule release, and clot retraction processes.
4. Prostaglandin and Nitric Oxide Balance: Prostaglandins and nitric oxide (NO) play opposing roles in platelet activation. Prostaglandins, including TxA2, promote platelet activation, while NO acts as a vasodilator and inhibits platelet activation. The balance between these two molecules is critical in regulating platelet reactivity.
Fig. 2 Mechanisms of Platelet Activation
Platelet Related Kits
Related ELISA Kits
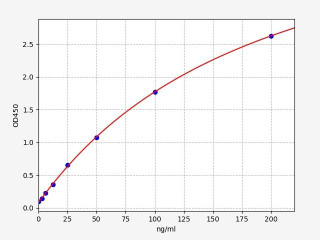
| Human TPO (Thrombopoietin) ELISA Kit | |
|---|---|
| ELISA Type: | Sandwich |
| Sensitivity: | 18.75pg/ml |
| Range: | 31.25-2000pg/ml |
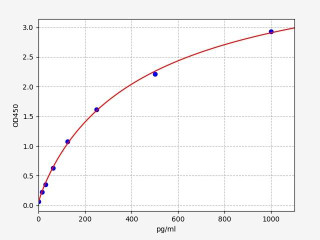
| Human PDGF AA / PDGF-A ELISA Kit | |
|---|---|
| ELISA Type: | Sandwich |
| Sensitivity: | 9.375pg/ml |
| Range: | 15.625-1000pg/ml |
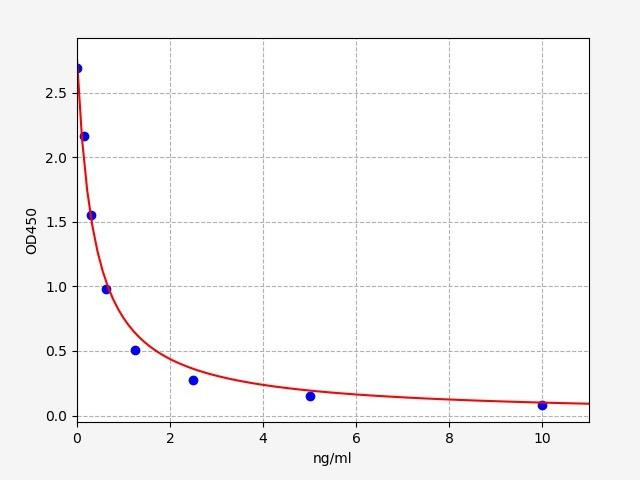
| PAF(Platelet Activating Factor) ELISA Kit | |
|---|---|
| ELISA Type: | Competitive |
| Sensitivity: | 0.094 ng/ml |
| Range: | 0.156-10 ng/mL |
Platelet Dysfunction:
Platelet dysfunction refers to abnormalities in the function or number of platelets, which can lead to bleeding or clotting disorders. Understanding platelet dysfunction is crucial for diagnosing and managing various hematological conditions.
Normal Platelet Levels:
In a healthy adult, the normal platelet count typically ranges between 150,000 to 450,000 platelets per microliter (μL) of blood. Within this range, platelets function optimally, contributing to hemostasis and wound healing by forming blood clots in response to vascular injury.
High Platelet Levels:
Thrombocytosis is a condition where the platelet count is elevated, usually exceeding 450,000 platelets per μL. High platelet levels can increase the risk of abnormal blood clot formation, leading to thrombosis. In some cases, excessive platelet count may cause blood flow obstruction, leading to circulation issues. It can be categorized into two types:
Essential Thrombocythemia/ Primary Thrombocytosis:
In primary thrombocytosis, the bone marrow produces an excessive number of platelets without an apparent underlying cause. This condition is often diagnosed incidentally during routine blood tests.
Secondary Thrombocytosis:
Secondary thrombocytosis occurs as a reactive response to various conditions, such as inflammation, infections, iron deficiency, certain cancers, and postsurgical recovery.
Low Platelet Levels (Thrombocytopenia):
Thrombocytopenia is a condition characterized by a decreased number of platelets in the blood, usually below 150,000 platelets per μL. Low platelet levels can result from various factors, including:
1. Decreased Platelet Production: Bone marrow disorders, such as aplastic anemia or leukemia, can lead to reduced platelet production.
2. Increased Platelet Destruction: Immune-mediated conditions, like immune thrombocytopenic purpura (ITP), can cause the immune system to destroy platelets.
3. Medications: Certain drugs, such as antibiotics or chemotherapy agents, can induce thrombocytopenia as a side effect.
Low platelet levels can result in a higher risk of bleeding, characterized by symptoms like easy bruising, petechiae (small red or purple spots on the skin), and prolonged bleeding after minor injuries.
Other Platelet-Related Disorders:
1. Thrombocytopathy: Thrombocytopathy refers to a group of platelet function disorders, where platelets do not function properly. This can result from inherited or acquired abnormalities in platelet receptors or signaling pathways, leading to impaired platelet adhesion, aggregation, or secretion.
2. Bernard-Soulier Syndrome: This is a rare genetic disorder characterized by a deficiency of glycoprotein Ib-IX-V complex on the platelet surface, resulting in abnormal platelet adhesion and bleeding tendencies.
3. Glanzmann Thrombasthenia: Glanzmann thrombasthenia is an inherited disorder caused by a deficiency of glycoprotein IIb/IIIa receptors on platelets, leading to impaired platelet aggregation and clot formation.
4. Gray Platelet Syndrome: Gray platelet syndrome is a rare genetic disorder characterized by the absence of alpha granules in platelets, resulting in mild to moderate bleeding tendencies.
5. May-Hegglin Anomaly: This is a rare inherited platelet disorder characterized by large platelets with Döhle-like bodies and mild to moderate bleeding tendencies.
Platelet Transfusion
Platelet transfusion is a clinical procedure that raises platelet levels in patients with low platelet counts or dysfunction. Platelets are collected from donors, processed into a concentrated product, and then infused into the recipient's bloodstream. This procedure is indicated for severe thrombocytopenia, platelet dysfunction, hematologic cancers, trauma, and major surgeries to prevent bleeding and support hemostasis.
Risks and Benefits:
Platelet transfusions are generally safe but carry potential risks, including transfusion reactions, TRALI, and allergic responses. The benefits of platelet transfusions often outweigh the risks, making it an essential medical intervention to manage platelet-related disorders and control bleeding during critical situations.
Conclusion
Platelets, the unassuming heroes of our circulatory system, may be small, but their significance is enormous. As we conclude this exploration into the world of platelets, we have witnessed their complex structure, their pivotal role in blood clotting, and their contributions to immune responses. From managing normal platelet levels to addressing platelet-related disorders, medical science continues to rely on these remarkable cellular fragments to safeguard our health. As we navigate the intricate interplay of platelets within our body, let us cherish the wonders of these unheralded components, forever indebted to their unwavering dedication in maintaining our cardiovascular well-being.
Written by Rithika Suresh
Rithika Suresh completed her undergraduate degree in Biotechnology in Anna University before completing her masters in Biotechnology at University College Dublin.
Recent Posts
-
Metabolic Exhaustion: How Mitochondrial Dysfunction Sabotages CAR-T Cell Therapy in Solid Tumors
Imagine engineering a patient's own immune cells into precision-guided missiles against cancer—cells …8th Dec 2025 -
The Powerhouse of Immunity: How Mitochondrial Fitness Fuels the Fight Against Cancer
Why do powerful cancer immunotherapies work wonders for some patients but fail for others? The answe …5th Dec 2025 -
How Cancer Cells Hijack Immune Defenses Through Mitochondrial Transfer
Imagine a battlefield where the enemy doesn't just hide from soldiers—it actively sabotages their we …5th Dec 2025




