Personalized Vaccines in Cancer Treatment: The Future of Immunotherapy
What Are Personalized Cancer Vaccines?
Personalized cancer vaccines are a cutting-edge approach in cancer treatment that are designed to activate a patient's immune system against their specific tumor. Unlike traditional vaccines that target infectious agents, personalized cancer vaccines are tailored to each individual's unique tumor characteristics. These vaccines are customized to exploit the specific genetic mutations and alterations present in the patient's tumor cells.
How Do Personalized Cancer Vaccines Work?
Personalized cancer vaccines work by utilizing neoantigens, which are mutated proteins expressed on the surface of cancer cells. These neoantigens serve as distinctive markers that differentiate cancer cells from healthy cells. The process begins by identifying the specific neoantigens present in the patient's tumor through genetic analysis. Once these neoantigens are identified, the patient's immune cells, particularly dendritic cells, are collected.
The collected dendritic cells are then loaded with the patient-specific neoantigens in the laboratory. This step educates the dendritic cells to recognize and target the cancer cells bearing these unique markers. Once the personalized vaccine is prepared, it is administered back to the patient. The vaccine activates the patient's immune system, particularly T cells, by presenting the neoantigens to these immune cells. As a result, the T cells are trained to recognize and attack the cancer cells expressing the specific neoantigens, leading to a targeted immune response against the tumor.
Types of Tumor Neoantigens
Neoantigens are tumor-specific antigens that are not present in normal cells and are generated as a result of mutations in the tumor cell genome. These mutations can lead to the creation of new proteins or changes in the structure of proteins that are recognized by the immune system as foreign, prompting an immune response against them. These neoantigens are absent in healthy cells, making them ideal targets for personalized cancer vaccines.
There are two main types of neoantigens: tumor-specific antigens (TSAs) and tumor-associated antigens (TAAs). TSAs are generated when tumor cells produce proteins that are not found on healthy cells. In contrast, TAAs are found on both tumor cells and healthy cells, but tumor cells typically produce higher levels of TAAs compared to healthy cells.
Neoantigens can be further classified into three categories: public, private, and shared neoantigens.
Public neoantigens are found in all tumor cells of a specific type. For example, the protein MART-1 (Melan-A) is a public neoantigen that is expressed by all melanoma cells. Public neoantigens are valuable targets for personalized cancer vaccines as they are consistently present across the tumor population, allowing for a broader immune response against the tumor.
Private neoantigens are unique to certain subsets of tumor cells within a specific tumor type. These neoantigens arise from mutations that are specific to individual tumor cells, making them distinct from other cells within the same tumor or other patients with the same cancer type. An example of a private neoantigen is the BRAF V600E mutation, which is found only in some melanoma cells. Designing personalized vaccines that target private neoantigens can address the heterogeneity of tumors and enhance the immune response against the specific subset of tumor cells harboring these mutations.
Shared neoantigens are found in tumors of different types. These neoantigens can be present in various cancer types, allowing for the development of broad-spectrum cancer vaccines. An example of a shared neoantigen is the protein NY-ESO-1, which is found in different tumor types, including melanoma, ovarian cancer, and bladder cancer. Targeting shared neoantigens opens up possibilities for developing vaccines that can be effective across multiple cancer types, potentially benefiting a broader range of patients.
Cancer Vaccines and Tumor Antigen Delivery
Cancer Vaccine Related Kits
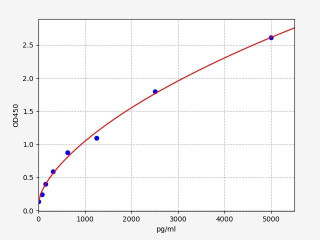
| Human Melan-A / MART-1 ELISA Kit | |
|---|---|
| ELISA Type | Sandwich |
| Sensitivity | 46.875pg/mll |
| Range | 78.125-5000pg/ml |
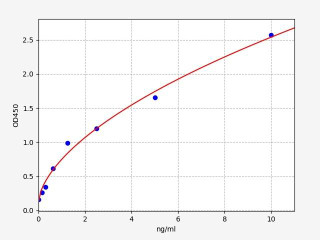
| Human NY-ESO-1 (Cancer/testis antigen 1) ELISA Kit (HUFI03454) | |
|---|---|
| ELISA Type | Sandwich |
| Sensitivity | 0.094ng/ml |
| Range | 0.156-10ng/ml |
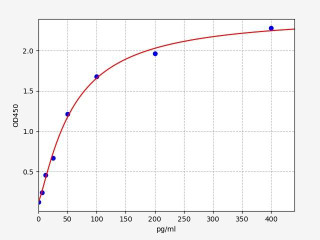
| Human PD-L1 / CD274 ELISA Kit | |
|---|---|
| ELISA Type | Sandwich |
| Sensitivity | 3.75pg/ml |
| Range | 6.25-400pg/ml |
Overview of Personalized mRNA and Peptide Cancer Vaccines
Personalized mRNA and peptide vaccines have emerged as promising strategies in the field of cancer immunotherapy. mRNA vaccines are made from pieces of genetic code (mRNA) that encode for tumor neoantigens. These vaccines can be used to target public, private, or shared neoantigens, making them highly customizable to the individual patient's tumor characteristics. On the other hand, peptide vaccines are made from peptides found on tumor cells. These vaccines utilize tumor proteins that are processed and presented by antigen-presenting cells to the immune system. Peptide vaccines primarily target public neoantigens.
Both mRNA and peptide vaccines have demonstrated promise in early clinical trials. However, there are challenges that need to be addressed before these vaccines can be widely used in clinical practice. For instance, their efficacy in advanced cancer patients who have developed resistance to immunotherapy remains uncertain. Additionally, the manufacturing process for these vaccines is labor-intensive and expensive. Despite these challenges, personalized cancer vaccines offer immense potential for the future of cancer treatment. These vaccines are tailored to each individual patient, allowing for a more precise and targeted approach. They hold the promise of providing long-lasting immunity against tumor cells. Continued research and development are essential to overcome the current obstacles and pave the way for the integration of personalized cancer vaccines as a standard part of cancer treatment in the future.
Written by Lauryn McLoughlin
Lauryn McLoughlin completed her undergraduate degree in Neuroscience before completing her masters in Biotechnology at University College Dublin.
Recent Posts
-
Enavatuzumab: Revolutionizing Cancer Research Through Novel Therapeutics
Quick Facts About EnavatuzumabWhat is Enavatuzumab?Enavatuzumab is a monoclonal antibo …17th Dec 2025 -
Alemtuzumab: Mechanism, Applications, and Biosimilar Advancements
Quick Facts About AlemtuzumabWhat is Alemtuzumab?Alemtuzumab is a monoclonal antibody …17th Dec 2025 -
Validation of MycoGenie Rapid Mycoplasma Detection Kit - A highly sensitive visual determination method for Mycoplasma detection.
The MycoGenie Rapid Mycoplasma Detection Kit enables the detection of 28 Mycoplasma sp …3rd Mar 2025




