C reactive protein
Delve into the world of C-reactive protein (CRP), a critical player in the body's response to inflammation, and understand its role in health and disease.
Key Takeaways
- C-reactive protein (CRP) is a marker of inflammation, increasing in response to infection, injury, or tissue damage.
- Produced by the liver, it's regulated by IL-6 and involved in immune responses.
- CRP's functions include pathogen recognition, opsonization, activating the complement system, and modulating inflammation.
- Used as a diagnostic biomarker, CRP levels help assess inflammation and cardiovascular risk.
- Elevated CRP levels are associated with various conditions, including infections, autoimmune diseases, and cancer.
What is C Reactive Protein?
C-reactive protein (CRP) is an acute-phase reactant, which means its levels increase in response to inflammation in the body. It is an important component of the immune system's response to infection, injury, or tissue damage.
The CRP (C-reactive protein) name is derived from the fact that it was first discovered in people with acute inflammation, whose blood reacted to the pneumococcal capsular polysaccharide (C-polysaccharide).
CRP is a hepatic acute-phase protein that increases after activation by macrophages and T cells. Its physiological role is to bind to lysophosphatidylcholine, which is present on the surface of dead or dying cells in order to activate the complement system via C1q. Measuring CRP levels in the blood is a common clinical practice to assess the presence and severity of inflammation in various diseases and conditions, as mentioned earlier. High levels of CRP can indicate the presence of an underlying inflammatory process, although it doesn't specify the cause or location of the inflammation.
CRP Gene and Structure
The gene responsible for producing CRP is called CRP, which is located on chromosome 1 (1q23.2). The expression of the CRP gene is regulated by various factors, including pro-inflammatory cytokines such as interleukin-6 (IL-6), which is released during inflammation.
C-reactive protein (CRP) is a pentameric protein, meaning it is composed of five identical subunits held together by noncovalent bonds. Each subunit consists of 206 amino acids and has a molecular weight of approximately 23 kilodaltons (kDa). CRP has a disc-shaped structure with a central pore. The protein subunits arrange themselves in a cyclic pattern, forming a ring-like structure. The central pore allows for interactions with various ligands and contributes to the protein's functional properties.
Structure of C-Reactive Protein Pentamer. Source: PDB
CRP Production
Acute phase response such as CRP are released in response to an increase in IL-6 levels, which are produced by macrophages and adipocytes in reaction to a variety of acute and chronic inflammatory stimuli such as bacterial, viral, or fungal infections, rheumatic and other inflammatory diseases, malignancy, and tissue injury and necrosis.
CRP, or C-reactive protein, is primarily produced by the liver in response to signals of inflammation. The process starts with an inflammatory stimulus such as infection or tissue damage, which triggers the release of pro-inflammatory cytokines like interleukin-6 (IL-6). IL-6 circulates in the bloodstream and binds to receptors on hepatocytes, liver cells. This binding activates specific genes, including the CRP gene. The CRP gene is transcribed into messenger RNA (mRNA), which serves as a template for protein synthesis. Within the liver cells, the mRNA is translated into CRP protein. The newly synthesized CRP protein is then released into the bloodstream, where it becomes measurable in blood tests. The production of CRP is relatively rapid, and its levels in the blood increase within a few hours of the inflammatory stimulus. Subsequently, when the inflammatory process subsides, CRP production decreases, and its levels gradually return to normal.
Production of CRP in response to bacterial infection.
CRP ELISA Kits
C-Reactive Protein Related Kits
| Human C Reactive Protein (CRP) ELISA Kit | |
|---|---|
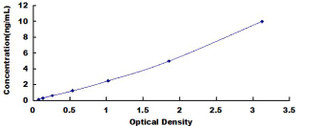
| ELISA Type | Sandwich |
| Sensitivity | 0.057ng/mL |
| Range | 0.156-10ng/mL |

| GeniePlex Human CRP/C-Reactive Protein Immunoassay | |
|---|---|
| ELISA Type | Multiplex |
| SKU: | HUAM00191 |
| Reactivity | Human |
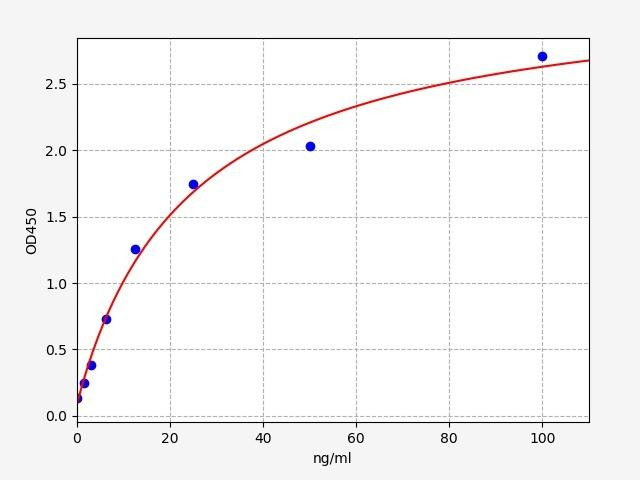
| Human Anti-CRP / Anti-C Reactive Protein ELISA Kit | |
|---|---|
| ELISA Type | Indirect ELISA |
| Sensitivity | 0.938ng/ml |
| Range | 1.563-100ng/ml |
Function of C Reactive Protein
C-reactive protein (CRP) serves several important functions in the body, particularly in the context of the immune response and inflammation.
- Recognition of Pathogens: CRP plays a role in the innate immune system by recognizing and binding to various molecules present on the surface of bacteria, viruses, and other pathogens. This binding helps facilitate their recognition and clearance by other components of the immune system.
2. Opsonization: CRP acts as an opsonin, which means it enhances the process of phagocytosis. By binding to pathogens, CRP marks them for uptake and destruction by immune cells called phagocytes, such as macrophages and neutrophils.
3. Activation of Complement System: CRP can activate the complement system, which is a group of proteins that participate in the immune response. When CRP binds to specific targets, it triggers a cascade of reactions leading to the activation of the complement system. This activation helps in the destruction and removal of pathogens.
4. Modulation of Inflammation: CRP can modulate the inflammatory response by interacting with immune cells and signaling molecules. It can stimulate the production of other pro-inflammatory cytokines, such as IL-6, and promote the recruitment of immune cells to the site of inflammation.
CRP as a Diagnostic Marker
CRP is a valuable biomarker for inflammation and infection. Monitoring CRP levels can help in the diagnosis and assessment of various conditions. Elevated CRP levels indicate the presence and severity of inflammation, and its decline indicates a response to treatment or resolution of the inflammatory process.
CRP Testing
High-Sensitivity CRP (hs-CRP) Test: This test measures CRP levels in the blood with high sensitivity, allowing for the detection of even low levels of CRP. It is often used for assessing cardiovascular risk and monitoring chronic inflammatory conditions.
hs-CRP testing has a greater sensitivity to detect even low levels of CRP accurately. It can measure CRP levels in a range as low as 0.1 mg/L, whereas conventional CRP testing has a lower limit of detection around 3 mg/L. This increased sensitivity allows for better discrimination and monitoring of subtle changes in CRP levels.
CRP Levels in blood
CRP levels are typically reported in milligrams per liter (mg/L) of blood. Normal CRP levels in healthy individuals are generally below 0.3 mg/dL. Elevated levels of CRP indicate the presence of inflammation, infection, or tissue damage. However, some healthy people have CRP levels of 10 mg/L or higher.
Several factors can impact C-reactive protein (CRP) concentrations in the bloodstream. Age, gender (with females often having slightly higher levels), obesity, lifestyle factors such as smoking and exercise, certain medications like statins and NSAIDs, hormonal changes, genetic variations, and the presence of specific health conditions like cardiovascular disease, chronic kidney disease, and rheumatoid arthritis can all affect CRP levels.
CRP Half Life
However, the half-life of C-reactive protein (CRP) in the bloodstream is relatively short, ranging from 18 to 24 hours. The exact half-life can vary slightly between individuals.
Due to its relatively short half-life, CRP levels can change rapidly in response to inflammation or infection. It allows for the measurement of acute changes in CRP levels, such as during an acute infection or following an inflammatory stimulus. Conversely, when the inflammatory stimulus subsides, CRP levels decrease accordingly.
It's worth noting that while CRP has a short half-life, it can still be detected in the bloodstream for a longer period, especially during sustained inflammation. However, monitoring changes in CRP levels over time can provide valuable information regarding the response to treatment or the resolution of an inflammatory condition.
CRP Clinical Significance
CRP levels can vary depending on the underlying disease or condition. Elevated CRP levels are commonly associated with various diseases and conditions characterized by inflammation. However, it's important to note that CRP levels alone are not diagnostic and should be interpreted alongside other clinical findings.
1. Infections: Bacterial, fungal, or viral infections can cause an increase in CRP levels. The severity of the infection is generally proportional to the elevation of CRP. However, specific cutoffs for CRP levels may vary depending on the type and location of the infection. CRP levels can rise as much as 50 to 100 mg/L in just 4-6 hours in mild to severe inflammation or an injury like a skin infection, cystitis, or bronchitis.
2. Rheumatoid Arthritis (RA): RA is an autoimmune disease characterized by chronic inflammation in the joints. CRP levels are often elevated in individuals with active RA, and monitoring CRP can help assess disease activity and response to treatment.
3. Systemic Lupus Erythematosus (SLE): SLE is an autoimmune disease that can affect multiple organs and tissues. CRP levels may be elevated during disease flares and can serve as an indicator of inflammation and disease activity.
4. Inflammatory Bowel Disease (IBD): Conditions such as Crohn's disease and ulcerative colitis fall under the umbrella of IBD. Elevated CRP levels are often observed during active disease states and can help in monitoring disease activity and response to treatment.
5. Cardiovascular Disease (CVD): Elevated CRP levels have been associated with an increased risk of CVD, including coronary artery disease and stroke. However, CRP levels alone are not sufficient for diagnosing or predicting cardiovascular events and are typically considered in conjunction with other risk factors.
6. Obstructive Sleep Opnea (OSA): Obstructive sleep apnea (OSA), a sleep disorder characterized by recurrent breathing pauses during sleep, has been found to be associated with elevated levels of C-reactive protein (CRP). Higher CRP levels in individuals with OSA suggest the presence of chronic low-grade inflammation, which may contribute to the increased cardiovascular risk often seen in OSA patients.
7. APOE Mutations: C-reactive protein (CRP) levels have been studied in relation to the apolipoprotein E (APOE) gene mutation, specifically the APOE4 variant. It has been found that individuals carrying the APOE4 allele may have higher CRP levels compared to those without the APOE4 mutation. This association suggests a potential link between the APOE4 gene variant, inflammation, and increased risk of certain conditions, including cardiovascular disease and Alzheimer's disease.
C Reactive Protein and Cancer
C-reactive protein (CRP) levels have been studied in relation to cancer, and elevated CRP levels have been found to be associated with certain types of cancer. In a prospective cohort study on colon cancer risk associated with CRP levels, people with colon cancer had significantly higher average CRP levels than individuals without the disease. It's also worth noting that the CRP levels in both groups were well within the normal range for people without heart disease. However, these results may suggest that low inflammation levels are linked to a decreased risk of colon cancer, which agrees with previous research suggesting anti-inflammatory medications might lower colon cancer risk.
1. Cancer Diagnosis and Prognosis: Elevated CRP levels have been observed in various types of cancer, including lung, colorectal, breast, pancreatic, and ovarian cancers. High CRP levels at the time of cancer diagnosis may indicate the presence of inflammation and an unfavorable disease state. In some cases, elevated CRP levels have been associated with advanced disease stage and poorer prognosis. However, it's important to note that CRP levels alone are not sufficient for cancer diagnosis, and additional diagnostic tests are necessary for accurate evaluation and staging.
2. Cancer-Related Inflammation: Cancer-related inflammation plays a crucial role in tumor development, progression, and metastasis. The tumor microenvironment can trigger the release of pro-inflammatory molecules, leading to systemic inflammation and elevated CRP levels. Chronic inflammation can promote tumor growth, angiogenesis, and immunosuppression. Elevated CRP levels may reflect the presence of this underlying inflammation, which can contribute to cancer progression. Monitoring CRP levels during cancer treatment can also help assess response to therapy, as a decrease in CRP levels may indicate treatment effectiveness.
In a prospective cohort study on colon cancer risk associated with CRP levels, people with colon cancer had significantly higher average CRP levels than individuals without the disease. It's also worth noting that the CRP levels in both groups were well within the normal range for people without heart disease. However, these results may suggest that low inflammation levels are linked to a decreased risk of colon cancer, which agrees with previous research suggesting anti-inflammatory medications might lower colon cancer risk.
CRP and Cancer
C-reactive protein (CRP) is an important marker of inflammation in the body, with clinical significance in various conditions. CRP is primarily produced by the liver in response to pro-inflammatory signals, and its levels rise rapidly during inflammation, infection, or tissue damage. Monitoring CRP levels can aid in diagnosing and assessing the severity of infections, monitoring disease activity in inflammatory conditions, assessing cardiovascular risk, and evaluating treatment response. However, CRP levels should be interpreted in conjunction with other clinical findings and diagnostic tests, as they are influenced by factors such as age, gender, obesity, and underlying health conditions. Understanding the functions, production, and factors affecting CRP levels helps healthcare professionals utilize this biomarker effectively to inform diagnosis, treatment decisions, and patient management.
Written by Rithika Suresh
Rithika Suresh completed her undergraduate degree in Biotechnology in Anna University before completing her masters in Biotechnology at University College Dublin.
Recent Posts
-
Enavatuzumab: Revolutionizing Cancer Research Through Novel Therapeutics
Quick Facts About EnavatuzumabWhat is Enavatuzumab?Enavatuzumab is a monoclonal antibo …17th Dec 2025 -
Alemtuzumab: Mechanism, Applications, and Biosimilar Advancements
Quick Facts About AlemtuzumabWhat is Alemtuzumab?Alemtuzumab is a monoclonal antibody …17th Dec 2025 -
Validation of MycoGenie Rapid Mycoplasma Detection Kit - A highly sensitive visual determination method for Mycoplasma detection.
The MycoGenie Rapid Mycoplasma Detection Kit enables the detection of 28 Mycoplasma sp …3rd Mar 2025




