Cancer Metabolism: Tumorigenesis, Metabolic Therapy & The Warburg Effect
Cancer Metabolism is the mechanism by which cancer cells make energy in order for them to grow and spread. Even in the presence of oxygen, cancer cells increase glucose uptake and produce lactate, which is defined by the Warburg Effect. This article also discusses areas related to cancer metabolism such as Tumorigenesis and Metabolic Therapy.
What is Cancer Metabolism?
Cancer metabolism refers to the distinct metabolic characteristics and alterations observed in cancer cells that support their energy needs for growth, proliferation, and survival. This includes the preference for glycolysis, even in the presence of oxygen (Warburg effect), increased glucose uptake, altered mitochondrial function, dysregulated lipid and amino acid metabolism, and the generation of reactive oxygen species (ROS). Cancer metabolism plays a crucial role in tumorigenesis and offers potential targets for cancer treatment and prevention.
Normal Cell VS Cancer Cell
Cancer Metabolism within Tumorigenesis
Cancer metabolism is an essential aspect of tumorigenesis, the process by which a normal cell transforms into a cancerous cell. During tumorigenesis, cells undergo genetic mutations that drive uncontrolled growth and malignancy. These mutations can activate oncogenes, which promote cell growth, and inactivate tumor suppressor genes, which help regulate cell growth. The dysregulated growth of cancer cells is a result of the combined action of oncogenes and the loss of tumor suppressor gene function.
Cancer metabolism plays a crucial role in the initiation and promotion of tumorigenesis. The altered metabolic pathways in cancer cells provide the necessary energy and resources for the acquisition of malignant traits. One key feature is the Warburg effect, where cancer cells preferentially utilize glycolysis for energy production, even in the presence of oxygen. This metabolic adaptation supports the rapid growth and proliferation of cancer cells. Moreover, cancer metabolism contributes to the biosynthesis of macromolecules required for tumor development and creates a favorable tumor microenvironment.
Targeting cancer metabolism offers potential avenues for cancer treatment and prevention. Strategies can involve inhibiting enzymes involved in cancer metabolism, such as glycolytic inhibitors, to impede energy production in cancer cells. Gene therapy approaches can also be used to repair mutated genes that contribute to malignant growth. Additionally, exploiting the differences in energy production between cancer cells and normal cells can guide the development of drugs that selectively target cancer metabolism.
Glutaminolysis in Cancer
Glutaminolysis, the metabolism of glutamine, has emerged as a significant metabolic pathway in cancer cells. Glutamine, a non-essential amino acid, serves as a versatile nutrient that contributes to several aspects of cancer metabolism. Cancer cells often exhibit an increased dependence on glutamine to support their proliferation and survival.
In cancer metabolism, glutamine is utilized as a carbon and nitrogen source for the synthesis of macromolecules, including nucleotides, amino acids, and lipids. Glutamine-derived carbon can enter the tricarboxylic acid (TCA) cycle as α-ketoglutarate, replenishing intermediates for biosynthetic pathways. This process, known as anaplerosis, helps meet the high biosynthetic demands of rapidly dividing cancer cells.
Moreover, glutamine metabolism plays a crucial role in maintaining redox balance and cellular antioxidant defenses. Glutamine can serve as a precursor for glutathione, a key antioxidant molecule that protects cells from oxidative damage. By regulating the cellular redox state, glutaminolysis contributes to the survival and proliferation of cancer cells in the often-oxidative tumor microenvironment.
Several oncogenes and tumor suppressor genes are involved in the regulation of glutamine metabolism in cancer cells. For example, the oncogene MYC has been shown to enhance glutamine uptake and metabolism, promoting tumor growth. Conversely, tumor suppressor genes such as p53 and PTEN can modulate glutamine metabolism to exert tumor-suppressive effects.
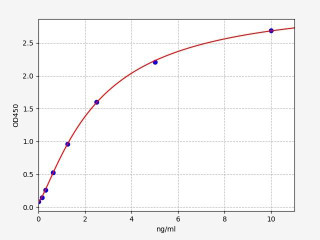
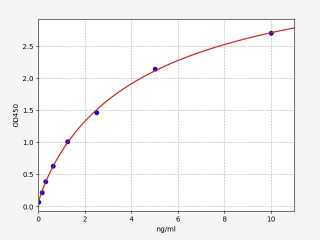
Cancer Metabolism Related Kits
Cancer Treatment - Metabolic Therapy
Metabolic therapy is a specialized approach in cancer treatment that focuses on targeting the altered metabolic processes of cancer cells. Cancer cells exhibit distinct metabolic characteristics and dependencies, making them vulnerable to interventions that exploit these differences. By selectively inhibiting key enzymes or pathways involved in cancer cell metabolism, metabolic therapy aims to disrupt the energy production and biosynthetic pathways necessary for cancer cell growth and proliferation, while minimizing harm to normal cells.
One primary target of metabolic therapy is glucose metabolism, specifically the Warburg effect, where cancer cells preferentially rely on glycolysis for energy production even in the presence of oxygen. Inhibitors of glycolysis have shown promise in impairing the energy production and biosynthetic pathways of cancer cells. Additionally, metabolic therapy explores targeting other metabolic pathways, such as energy production and the production of reactive oxygen species, which are vital for cancer cell survival and proliferation.
The development of metabolic therapy involves investigating a range of metabolic inhibitors that selectively target enzymes or pathways involved in cancer cell metabolism. Clinical trials are currently underway to evaluate the effectiveness and safety of these inhibitors as potential treatments for cancer. Furthermore, combining metabolic inhibitors with conventional therapies is being explored to enhance treatment outcomes through synergistic effects. Metabolic therapy holds great potential as a novel and targeted approach in cancer treatment, with ongoing research aiming to optimize therapeutic strategies and improve patient outcomes.
Metabolism in Cancer: The Warburg Effect
One of the hallmarks of cancer metabolism is the Warburg effect, a phenomenon first described by Otto Warburg in the 1920s. The Warburg effect refers to the observation that cancer cells preferentially rely on glycolysis, a process that converts glucose into lactate, even in the presence of sufficient oxygen. This metabolic alteration is a fundamental characteristic of many cancer types.
In normal cells, the primary pathway for energy production is oxidative phosphorylation, which occurs in the mitochondria and efficiently generates ATP. However, cancer cells exhibit a metabolic switch, favoring glycolysis as the primary energy-generating pathway. Despite the lower energy yield compared to oxidative phosphorylation, glycolysis provides several advantages to cancer cells.
First, glycolysis allows cancer cells to rapidly generate ATP, providing the energy needed for their accelerated growth and proliferation. This high rate of glycolysis also facilitates the production of metabolic intermediates required for the synthesis of macromolecules, including nucleotides, amino acids, and lipids, necessary for cell division and biomass accumulation.
Another advantage of glycolysis is its ability to operate under conditions of limited oxygen supply, commonly found within the tumor microenvironment. By relying on glycolysis, cancer cells can survive and thrive in low-oxygen (hypoxic) conditions, which would be detrimental to normal cells relying on oxidative phosphorylation.
The molecular mechanisms underlying the Warburg effect are complex and multifaceted. Several oncogenes and tumor suppressor genes, such as MYC, HIF-1α, and p53, play crucial roles in modulating the expression of key enzymes involved in glycolysis and mitochondrial metabolism. Additionally, altered signaling pathways, such as the PI3K/AKT/mTOR pathway, contribute to the metabolic reprogramming observed in cancer cells.
Schematic of The Warburg Effect
Metabolic Adaptations in the Tumor Microenvironment
The tumor microenvironment exerts profound effects on cancer cell metabolism, influencing tumor behavior and progression. Within this dynamic ecosystem, cancer cells adapt to altered nutrient availability, hypoxia, and interactions with stromal cells.
Metabolic adaptations within the tumor microenvironment include increased glucose and amino acid uptake to fuel energy production and biosynthesis. Hypoxia triggers the activation of hypoxia-inducible factor 1, promoting glycolytic metabolism and angiogenesis. Interactions with stromal cells, such as cancer-associated fibroblasts and tumor-associated macrophages, further shape the metabolic landscape.
These metabolic adaptations support tumor growth and contribute to treatment resistance. Understanding the metabolic alterations in the tumor microenvironment provides insights into potential therapeutic opportunities. Targeting nutrient availability, metabolic interactions, or hypoxia-induced pathways may present novel approaches to overcome treatment resistance and improve outcomes. Ongoing research aims to develop personalized cancer therapies based on these metabolic adaptations.
Written by Lauryn McLoughlin
Lauryn McLoughlin completed her undergraduate degree in Neuroscience before completing her masters in Biotechnology at University College Dublin.
Recent Posts
-
Enavatuzumab: Revolutionizing Cancer Research Through Novel Therapeutics
Quick Facts About EnavatuzumabWhat is Enavatuzumab?Enavatuzumab is a monoclonal antibo …17th Dec 2025 -
Alemtuzumab: Mechanism, Applications, and Biosimilar Advancements
Quick Facts About AlemtuzumabWhat is Alemtuzumab?Alemtuzumab is a monoclonal antibody …17th Dec 2025 -
Erenumab: Transforming Migraine Prevention Through CGRP Receptor Inhibition
Quick Facts About ErenumabWhat is Erenumab?Erenumab is a fully human monoclonal antibo …1st Apr 2025