CD8+ T Cells: Understanding the Role of Cytotoxic T Cells in Immunity
CD8+ T cells, also known as cytotoxic T lymphocytes (CTLs), are a critical component of the immune system. They play a vital role in defending the body against viral infections, intracellular pathogens, and tumor cells. This article will delve into the biology of CD8+ T cells, their mechanisms of action, and their clinical relevance, particularly in immunotherapy and infectious disease control.
What Are CD8+ T Cells?
CD8+ T cells are a subset of T lymphocytes that express the CD8 glycoprotein on their surface. This marker distinguishes them from other T cells, such as CD4+ helper T cells. CD8+ T cells are often referred to as killer T cells because of their ability to recognize and destroy infected or cancerous cells.
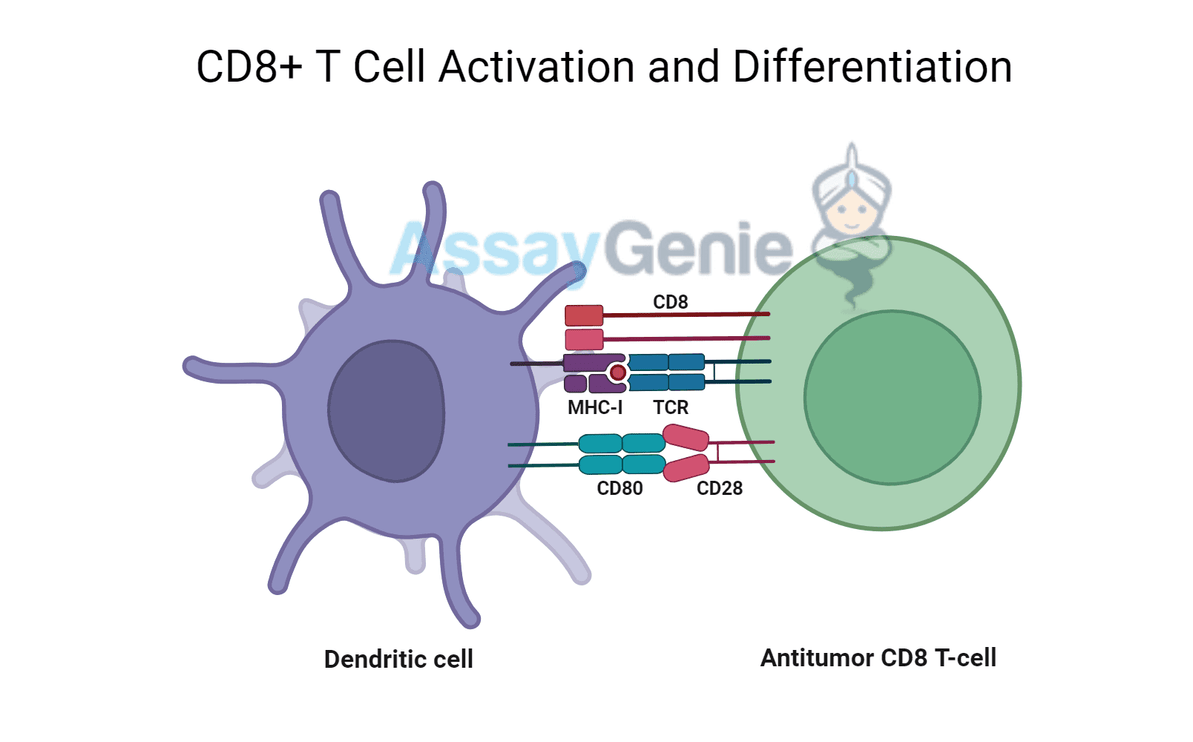
Differentiation and Activation
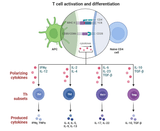
CD8+ T cells are initially naive when they emerge from the thymus. They require antigen presentation by antigen-presenting cells (APCs), typically dendritic cells, for activation. The key to their activation lies in recognizing foreign antigens presented by MHC Class I molecules on the surface of infected cells. This interaction, along with costimulatory signals, drives their differentiation into effector cytotoxic T cells.
Step | Description |
|---|---|
Antigen Recognition | CD8+ T cells recognize antigens bound to MHC Class I. |
Costimulation | Costimulatory signals enhance activation (e.g., CD28). |
Cytotoxic Effector Phase | CD8+ T cells differentiate and acquire cytotoxic functions. |
Mechanisms of Cytotoxicity
Once activated, CD8+ T cells execute their primary function: killing infected or abnormal cells. This process involves multiple pathways and effector molecules.
Direct Killing Through Perforin and Granzymes
1. Perforin-Granzyme Pathway:
2. Fas-FasL Pathway:
- CD8+ T cells express Fas Ligand (FasL), which binds to Fas receptors on target cells, triggering a cell death signal.
Cytotoxic Pathway | Mechanism |
|---|---|
Perforin-Granzyme | Perforin forms pores, and granzymes induce apoptosis. |
Fas-Fas Ligand Interaction | FasL on T cells binds Fas receptors, triggering cell death. |
Cytokine Secretion
In addition to direct killing, CD8+ T cells secrete cytokines that enhance the immune response. These include:
- Interferon-gamma (IFN-γ): Promotes macrophage activation and enhances MHC expression, increasing immune surveillance.
- Tumor Necrosis Factor-alpha (TNF-α): Contributes to apoptosis and inflammation.
CD8+ T Cells in Viral Infections
Examples of Viral Targets
Virus | Role of CD8+ T Cells |
|---|---|
HIV | Control viral load by killing infected cells, but virus evades CTLs. |
Influenza | Clear infected cells during the acute phase of infection. |
Memory CD8+ T Cells
After an infection is resolved, some CD8+ T cells become memory cells. These long-lived cells remain in the body, ready to rapidly respond to future infections by the same pathogen.
CD8+ T Cells and Cancer Immunity
CD8+ T cells are central to the immune system's ability to detect and destroy tumor cells. Tumor cells often present tumor-associated antigens (TAAs) via MHC Class I molecules. CD8+ T cells can recognize these antigens and kill the tumor cells, playing a vital role in immune surveillance and cancer immunotherapy.
Tumor Immune Evasion
Tumors develop mechanisms to evade immune detection, such as:
- Downregulation of MHC Class I molecules: Reducing the visibility of tumor antigens to CD8+ T cells.
- Immunosuppressive environments: Tumors secrete cytokines like TGF-β that inhibit CD8+ T cell function.
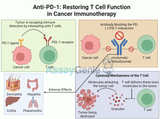
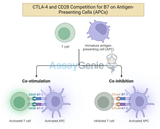
Immunotherapy: Enhancing CD8+ T Cell Function
In cancer treatment, immunotherapies such as checkpoint inhibitors (e.g., anti-PD-1, anti-CTLA-4) boost CD8+ T cell activity. These therapies block inhibitory signals that limit T cell activation, enabling CD8+ T cells to effectively target tumors.
Checkpoint Inhibitor | Mechanism of Action |
|---|---|
Anti-PD-1 | Blocks PD-1, allowing sustained CD8+ T cell activity. |
Anti-CTLA-4 | Increases T cell activation by blocking inhibitory signals. |
CD8+ T Cells in Immunotherapy
The therapeutic use of CD8+ T cells has garnered significant attention in recent years. Several approaches are currently in use or under development to enhance their cytotoxic potential against diseases such as cancer.
Adoptive T Cell Transfer (ACT)
Adoptive T cell transfer involves isolating T cells from a patient, expanding them in the lab, and reintroducing them into the body to fight cancer. Chimeric Antigen Receptor (CAR) T cell therapy is a form of ACT where T cells are genetically modified to target specific antigens on tumor cells.
Immunotherapy Type | Description |
|---|---|
Checkpoint Inhibitors | Enhance CD8+ T cell activity by blocking inhibitory pathways. |
Adoptive T Cell Transfer (ACT) | T cells are expanded and reinfused to target cancer cells. |
CAR-T Cell Therapy | T cells are genetically modified to target specific tumor antigens. |
Therapeutic Vaccines
Conclusion
CD8+ T cells are pivotal in both fighting infections and combating cancer. Their ability to recognize and destroy infected or abnormal cells makes them a critical component of the immune system. The use of CD8+ T cells in immunotherapy, particularly through checkpoint inhibitors and adoptive T cell transfer, has revolutionized the treatment of several cancers. However, challenges remain in overcoming tumor immune evasion and enhancing memory responses. Ongoing research continues to expand our understanding of CD8+ T cells and their therapeutic potential.
References
Recent Posts
-
CD4+ T Cells: Unveiling the Role of Helper and Regulatory T Cells
CD4+ T cells are central to the immune system, functioning as coordinators of immune r …25th Sep 2024 -
Anti-PD-1: Restoring T Cell Function in Cancer Immunotherapy
Cancer immunotherapy has revolutionized the treatment landscape for various malignanci …24th Sep 2024 -
Anti-CTLA-4: Unleashing the Power of T Cells in Combination Immunotherapy
Immunotherapy has revolutionized cancer treatment by harnessing the body's immune syst …24th Sep 2024